by Jeffrey J. Downey, attorney and advocate for Elders in our long-term care system.
On the web at Jeffdowney.com
Phone: 703-564-7318, 703-564-7336
Serving clients in Virginia, Maryland and Washington DC.
Download the full article with citations here.
A. Impact in the United States
Its estimated that some 2.5 million patients develop pressure wounds (a/k/a bed sores) every year, in both hospitals and rehab facilities, costing the US taxpayers an estimated 9 to 11 billion dollars a year. More than 60,000 patients die annually from pressure wounds. Medicaid has estimated that each pressure wound adds $43,180 in costs to a patient’s hospital stay.
While the monetary losses are significant, equally important is the fact that pressure wounds adversely impact a patient’s quality of life and mortality. Elders who develop open wounds often develop infections and other complications that can severely limit or end their quality of life.
B. Causes and Staging of Pressure Wounds
As the term suggests, a pressure wound (or decubitus ulcer) is caused by unrelieved pressure that compromises the skin and underlying tissue to the point where reduced blood flow causes tissue death. Often these wounds develop when patients have reduced mobility or fragility. Their development is often a sign of nursing neglect. Compromised nutrition and immobility are important risk factors that have to be addressed for all high-risk patients.
As observed by one author on the subject, “the treatment and care of chronic wounds may be an unglamorous aspect of medical practice, but for both the patient and the society, the resulting morbidity and cost are considerable. Indeed much of the medical establishment, whether through lack of confidence, training, interest, or remunerative potential, continues to perceive this to be under the province of someone else.” Evidence Based Management Strategies for Treatment of Chronic Wounds. F. Werken, MD, Mayer Tennenhus, MD
Medicare changed reimbursement rules to deny reimbursement to hospitals and other providers who allow pressure wounds to develop on their watch. This change in reimbursement policy is part of a broader realization that these outcomes are avoidable and healthcare providers who allow such conditions to develop will be held accountable – as they should. But such regulatory changes have also resulted in new facility practices designed to disguise pressure ulcers as other types of wounds. Facilities may not stage the wound or they may under stage the wound.
1. Medicare Definitions of Staging:
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
Intact skin with a local area of area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. - Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis
Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible and deeper tissues are not visible. Granulation tissue, slough and eschar are not present. - Stage 3 Pressure Injury: Full-thickness skin loss
Full-thickness loss of skin, in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. - Stage 4 Pressure Injury: Full-thickness skin and tissue loss
Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole (rolled edges), undermining and/or tunneling often occur. Depth varies by anatomical location. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury. - Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss
Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar (i.e. dry, adherent, intact without erythema or fluctuance) on an ischemic limb or the heel(s) should not be removed.
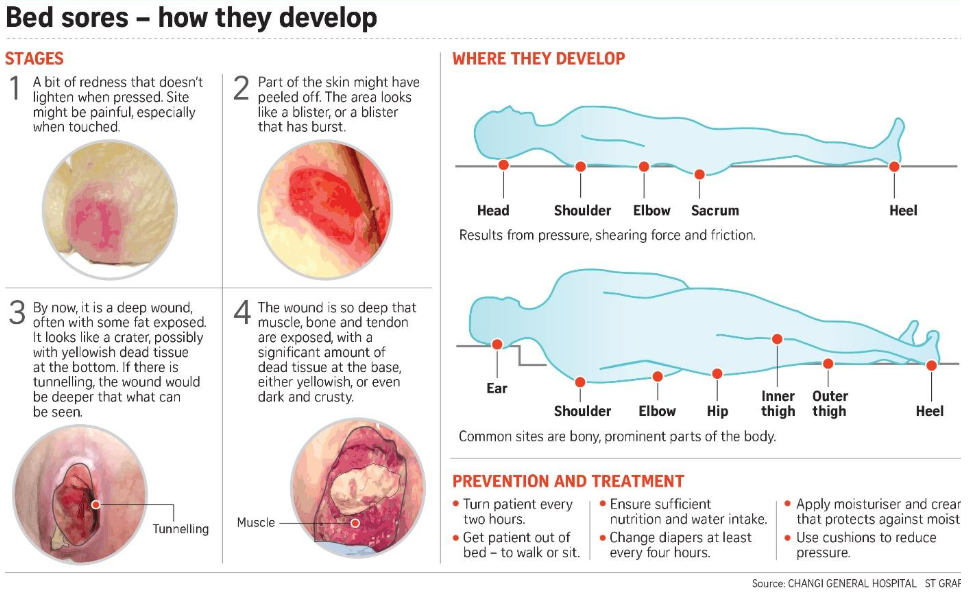
Pressure sores, also called bed sores or decubitus ulcers are most common on pressure points like the sacrum, elbows or heels. Here is a list of common pressure areas:
- sacrum (lower back)
- coccyx (tailbone)
- heel of the foot
- ischium (the base of the buttocks, “seat bones”)
- trochanter (hip, from lying on side, something rubbing, or tight clothes)
- elbow (from leaning on it)
- knee (from spasms or side-lying with one knee on top of other)
- ankle (from lying on side)
- toes and bony areas of foot (from tight-fitting shoes)
- back of the head
C. Best Practices for Prevention – Following the Guidelines
Unlike some mysterious illness or incurable disease, the causes of decubitus ulcers and methods of prevention are well known to the industry. However, since their prevention in high risk patients is complex and labor intensive, a systematic approach is required to consistently offload (reduce) pressure and coordinate other disciplines, like dietary and rehab departments.
Hospitals and rehab facilities need to place a strong emphasis on quality improvement. There are great resources providing tools and recommendations for reducing the incidence of pressure wounds. Preventing Pressure Ulcers in Hospitals, a toolkit for improving quality of care. Recommendations include, inter alia, complete body checks every shift, use of a turning and repositioning schedule and repositioning as often as every hour for patients who are completely immobile. Frequent reassessment is required to change any care plan that is not working to increase offloading frequency and evaluate other modalities, like an air fluidized bed.
Independently evaluating and treating any nutritional deficiencies is a critical part of any prevention or treatment regimen. Pressure Ulcer and Nutrition, S. Saghalieine, Kasra Dehgman. This author explains that increased needs for energy, protein, zinc, and Vitamins A, C, and E and also amino acids such as arginine and glutamine have been well documented in the literature. Hydration plays a vital role in the preservation and repair of skin integrity. Dehydration, a common problem in the elderly population, disturbs cell metabolism and wound healing.
Some best practices are well documented in National and European guidelines:
1. National Pressure Ulcer Advisory Panel (NPUAP) And European Pressure Ulcer Advisory Panel (EPUAP) Pressure Ulcer Prevention And Treatment Clinical Practice Guideline, Second Printing, February 2010 (Download Article)
- This guideline recommends: “record repositioning regimes, specifying frequency and position adopted, and include an evaluation of the outcome of the positioning regime. … Documentation provides a written record of care delivery and, as such, serves as evidence that repositioning has occurred. It is therefore important to record each repositioning episode and include a record of the individual’s skin condition as an indicator of tolerance of that particular positioning plan.”
- Although not specifying a specific turning and repositioning frequency, the guideline suggests that “frequent assessment of the individual’s skin condition will help to identify the early signs of pressure damage and, as such, her/his tolerance of the planned repositioning schedule. If changes in skin condition should occur, the repositioning care plan needs to be reevaluated.”
- The guideline specifies that nursing staff should “continue to turn and reposition, where possible, all individuals at risk of developing pressure ulcers. Repositioning is still required for pressure relief and comfort when a support surface is in use. The use of a support surface is, therefore, not a justification for discontinuing the use of repositioning.”
- If pressure ulcers are not healing: re-evaluate the individual and his/her pressure ulcers, intensify prevention strategies as indicated, [and] consider changing the support surface to improve pressure redistribution, shear reduction, and microclimate control matched to the individual’s needs.”
- The guideline emphasizes that nursing staff should limit the time an individual spends seated in a chair without pressure relief.
2. National Pressure Ulcer Advisory Panel (NPUAP), European Pressure Ulcer Advisory Panel (EPUAP) and Pan Pacific Pressure Injury Alliance Prevention and Treatment of Pressure Ulcers: Quick Reference Guide, Emily Haesler (Ed.). Cambridge Media: Perth, Australia; 2014
- For individuals at risk of pressure ulceration, a head-to-toe assessment with particular focus on skin overlying bony prominences is required. “Each time the patient is repositioned is an opportunity to conduct a brief skin assessment [16].” Every individual should be assessed for pressure ulcer risk within eight hours of admission [70].
- An individualized pressure ulcer prevention plan should be documented and implemented [70].
- “Repositioning of an individual is undertaken to reduce the duration and magnitude of pressure over vulnerable areas of the body and to contribute to comfort, hygiene, dignity, and functional ability.” In circumstances in which “regular positioning is not possible…. Because of their medical condition, and alternative prevention strategy such as providing a high specification mattress or bed may need to be considered [23].”
- Repositioning frequency must take into account the pressure redistribution support surface in use, tissue tolerance, general medical condition, overall treatment objectives, skin condition, comfort, and level of activity and mobility. “If changes in skin condition should occur, the repositioning care plan needs to be reevaluated [23].”
- “Limit the time an individual spends seated in a chair without pressure relief [25].”
- “Do not position an individual directly on a pressure ulcer [25].” Avoid seating an individual within ischial ulcer in a fully erect posture in chair or bed … The ischia bear intense pressure when an individual is seated [64].” Do not position the individual directly on a medical device unless it can not be avoided [32].
- “Continue to turn and reposition the individual regardless of the support surface in use…. No support surface provides complete pressure relief [25].”
- “If sitting in a chair is necessary for individuals with pressure ulcers on the sacrum/coccyx or ischia limit sitting to three times a day in periods of 60 minutes or less [26].” Those who are unable to reposition independently must be repositioned [57].
- Microshifts (“small shifts”) “do not replace selection of a more appropriate pressure redistribution support surface when needed or turning (major shifts in body position) [55].”
- An individual’s cognitive status must be considered when developing a pressure ulcer prevention and treatment plan [56].
- “Record repositioning regimes, specifying frequency and position adopted, and include an evaluation of the outcome of the positioning regimen. Documentation provides a written record of care delivery and, as such, serves as evidence that repositioning has occurred [26].” A repositioning schedule should be initiated as soon as possible after admission [55].
- In order to prevent heel pressure ulcers, “ensure that the heels are free of the surface of the bed… Heel suspension devices are preferable for long-term use, or for individuals who are not likely to keep their legs on the pillows… Remove the heel suspension device periodically to assess skin integrity [27].”
- For those individuals with existing pressure sores, “consider replacing the mattress with a support surface that provides more effective pressure redistribution, shear reduction, and microclimate control if he or she cannot be positioned off the existing pressure ulcer, has pressure ulcers on two or more turning surfaces… that limit turning options, [or] fails to heal or demonstrates ulcer deterioration [29].”
- A pressure redistributing seat cushion is recommended to prevent pressure ulceration.
- Pressure sores descriptions are to include location, stage, size, tissue type, color, the condition of the skin around the pressure sore, the wound edges, sinus tracts, undermining, tunneling, exudate, and odor.
- Pressure sore infection can be diagnosed if there is redness extending from the edge of the ulcer, induration, new or increase in pain or warmth, purulent drainage, an increase in size, fever, malaise, lymphadenopathy, confusion or delirium, anorexia, crepitus, fluctuance, and/or discoloration of the surrounding skin [42].
- Conduct regular evaluation of organizational performance in pressure ulcer prevention and treatment and provide this information as feedback to these stakeholders. There should be a tailored program of staff education and cues to perform pressure ulcer prevention. A facility should develop an education policy for pressure ulcer prevention and treatment at an organizational level.
D. Legal Rights and Remedies – Reporting deficient facilities.
Hospitals, nursing homes or assisted living facilities that allow their patients to develop pressure wounds are often subject to liability for such failures. Liability can take the form of regulatory violations by their licensing authority or a civil claim of malpractice/negligence. Often the civil case comes down to a battle between the experts as to whether the wound was avoidable or not. However, for a facility to credibly argue that the pressure wound is unavoidable, they must have first instituted and documented aggressive efforts at preventive care. A facility cannot allow a resident to lie in their own human waste, not being turned or cleaned, and argue that their wound was unavoidable.
Under Federal law nursing homes are obligated to prevent the development of all pressure wounds unless the patient suffers from a clinical condition that makes the development of such wound clinically unavoidable. As this is the unusual situation, the development of a pressure wound often creates malpractice liability for the facility that allowed the wound to develop.
In most states a victim who develops a pressure wound can obtain compensation for his/her injury, pain and suffering, inconvenience, lost wages and medical expenses. Should the pressure wound cause death, the surviving statutory beneficiaries have a claim for the death of their loved one that focuses on the loss to the beneficiaries (as opposed to the suffering of the victim). In Virginia one cannot recover both pain and suffering (survivorship claim) and wrongful death damages for the same injury. So, if a sacral pressure wound caused suffering which lead to the death of the patient, the Plaintiff, at some point, will be limited to only one form of damages. Where causation is disputed on the death claim, this becomes an issue for the jury to resolve.
Most states now have caps in non-economic damages, which limit recovery. In Virginia that cap section can be found at Va. Code § 8.01-581.15. As of July 2014, the cap is $2.15 million. It goes up 50,000 each year until it hits $2.95 million in 2030. The Virginia cap applies to both economic damages (medical bills, lost wages) and non-economic damages (pain, suffering, inconvenience)
The cap in Maryland as of 2018 is $800,000, but it is limited to non-economic damages. So, if you incurred lost wages or medical bills, they are not covered or limited by the cap. Where there are two or more beneficiaries in a wrongful death case, the cap rises to 1 million in non-economic damages.
42 CFR 483.25 (c)
Interpretive F-tag language for the above regulation explains 42 CFR 483.25 (c) and clarifies the definition of avoidable and unavoidable pressure ulcers. Avoidable means “that the resident developed a pressure ulcer and that the facility did not do one or more of the following: evaluate the resident’s clinical condition and pressure ulcer risk factors; define and implement interventions that are consistent with resident needs, resident goals, and recognized standards of practice; monitor and evaluate the impact of the interventions; or revise the interventions as appropriate.” Conversely, unavoidable means “that the resident developed a pressure ulcer even though the facility had evaluated the resident’s clinical condition and pressure ulcer risk factors; defined and implemented interventions that are consistent with resident needs, goals, and recognized standards of practice; monitored and evaluated the impact of the interventions; and revised the approaches as appropriate.
E. Protecting Your Rights
If you or a loved one have suffered an adverse outcome at a hospital or nursing home, it’s important to take immediate action to protect your rights. Consider doing the following:
- Do not sign any mandatory arbitration or jury trial waivers upon admission to any facility.
Rather than provide quality care, healthcare providers are increasingly seeking to limit your rights to file a claim should malpractice occur in their facility. This is done through the signing of a mandatory arbitration provision or other clause that prohibits the party subject to the neglect from filing a negligence or malpractice claim in Court. Healthcare providers push such cases into arbitration, where claimants often face an uphill battle because of increased costs and the fact that the case will no longer decided by a jury.
- After suffering an adverse event, wound or other injury, seek legal advice immediately. You do not have to hire a lawyer to seek guidance on what to do. Just call my office, 703-564-7318 or 703-564-7336. Your attorney will take steps to preserve evidence and if possible, opt out of any mandatory arbitration provisions that could limit your rights.
- Make notes, take photos and know your facts. It’s important to arm yourself with facts that might be important to prove your case. For example, was the facility turning your loved one every 1 to 2 hours? What was the nature of the wound before transfer to the hospital? Make sure you ask to see it and find out what the facility was supposed to be doing to prevent it. The best pressure wound cases are ones in which the family visited and could corroborate from their own observations that mom was not being cleaned and repositioned on a regular basis.
- Request records from the facility and review them. Sometimes a facility will try and put the blame back on the patient or the family. They may blame the patient for not cooperating in being moved or repositioned. But if your loved one had dementia or was immobile, he may not have been able to turn or reposition himself.
- Respond aggressively to the wound at its early stages. Sometimes a Stage I pressure wound (redness without a break in the skin) may not be a big deal if it develops on a healthy person. But where it appears on a pressure area of a nursing home patient who will be subject to ongoing pressure forces, it should be treated seriously. It’s easier to treat a wound at its early states, stage I or State II, before it becomes an open, infected wound. Once you are alerted to the existence of any wound, you need to educate yourself and become involved in the patient’s care. Attend care plan meetings and ask about the wound every day, which will help focus the staff on this issue. Ask about nutritional interventions to boost protein levels necessary for wound healing. If it appears infected or foul smelling, ask for a wound consult by an infectious disease doctor. If the patient is placed on antibiotics, request probiotics to restore the normal intestinal flora of the stomach.
- Report instances neglect to your licensing authority. But before you take this step, I would urge you to discuss this issue first with legal counsel, as I sometimes advise my clients not to file Dept of Health complaints where an investigation may not go anywhere because of the complexities or issues involved in the case. State Departments of Health that investigate nursing homes are often under resourced. They tend to only cite clear cut regulatory violations despite the reality that issues of neglect can often be complicated and nuanced because of the patient’s underlying medical condition.
F. Call to Action
Contact competent legal counsel to protect your rights. Unless people assert their rights to quality healthcare, those rights are often ignored. This is especially true in the long-term care setting, where nursing homes often staff their facilities leanly to increase profits.
If you or a loved one has developed a pressure wound or suffered other bad outcomes at nursing home, hospital or assisted living facility, call the Law Office of Jeffrey J. Downey for a free consultation. Mr. Downey has been representing elders in such cases for over 25 years and has a wealth of legal experience in this area. His large settlements and verdicts speak to the level of his commitment. His clients have testified before the United States Congress to expose nursing home neglect.
No attorney’s fees are charged unless there is a settlement or recovery, so call now for your free consultation.
Tags: Pressure sore attorney, pressure sore lawyer, abuse lawyer, attorney handling bed sores, decubitus ulcer attorney or lawyer, bed sore complaints, bed sore nursing home, nursing home lawyer, decubitus ulcers, bed sore attorney, bed sore lawyer, wound lawyer, nursing negligence attorney, pressure sore malpractice, bed sore neglect, neglect causing bed sores, attorney handling bed sore cases, sacral pressure wound, unavoidable pressure wound, avoidable pressure wound, Virginia bed sore attorney, Maryland bed sore attorney, Washington DC pressure sore attorney/lawyer
